Plantar Fasciitis
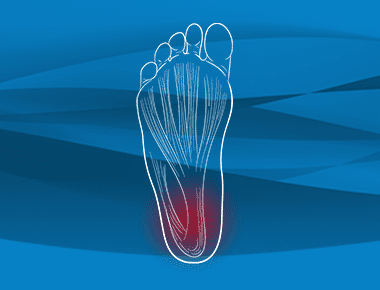
The plantar fascia is the most bottom superficial level of your foot. It’s a ligament that originates at the heel bone and goes all the way up to the ball of your foot. Plantar fasciitis occurs when that ligament becomes irritated and inflamed, resulting in pain and swelling in the bottom of the heel. Learn more about diagnosing and treating plantar fasciitis, and what to expect if you need treatment.
Hosted by Eric Chehab, MD
Episode Transcript
Episode 15 - Plantar Fasciitis
Dr. Eric Chehab:Welcome to Illinois Bone and Joint Institute’s OrthoInform, where we talk all things orthopedics, to help you move better, live better. I’m your host, Dr. Eric Chehab. With OrthoInform, our goal is to provide you with an in-depth resource about common orthopedic procedures that we perform every day.
Today it’s my pleasure to welcome Dr. Carla Gamez, who will be speaking about the dreaded plantar fascia. As a brief introduction, Dr. Gamez graduated from Boston College in 1990, with a degree in History and French. She earned her Master’s Degree of French Civilization at the Sorbonne University in Paris in 1992.
She earned her Bachelor’s of Science at Loyola in 1994. She then earned her degrees in Podiatric Medicine at the famous Dr. William M. Scholl School of Podiatric Medicine, right here in Chicago in 1998. And that Dr. William M. Scholl is the Dr. Scholl’s that we see on every pharmacy shelf in the country, is that correct?
Dr. Carla Gamez:
That is correct.
Dr. Eric Chehab:
Then she completed her podiatric surgical residency at the Midwestern Regional Medical Center in Zion, Illinois in 2000, where she served as chief resident. Dr. Gamez has practiced in the Chicago area for her entire career and has been with Illinois Bone and Joint institute since 2001.
She has been board certified in foot surgery since 2007, she has helped thousands of patients who suffer from painful foot conditions, and she is a kind caring and outstanding clinician and an equally good friend and colleague. So Carla, it’s a pleasure to have you here on OrthoInform.
Welcome, and thanks for being here today.
Dr. Carla Gamez:
Thanks, Eric. And thanks for having me.
Dr. Eric Chehab:
So let’s get right to it. I mean, I have to be honest with you, most of us wouldn’t even know that we have a plantar fascia, until we have a problem with it. And then we know, painfully, that it exists. That’s why I say dreaded. I’m at an age where I’ve had plantar fasciitis and I couldn’t believe how disabling it felt. And so what is the plantar fascia, and why is it so important to the function of the foot?
Dr. Carla Gamez:
Plantar fascia is the most bottom superficial level of your foot. And it’s a ligament that starts and originates at the heel bone. And it goes all the way up to the ball of your foot.
People don’t realize, one, that it’s that extensive, and people don’t realize it’s a ligament. People think it’s a tendon and we can’t move ligaments. We can move tendons. We can’t move ligaments. The ligament is a structural component of the foot. It is incredibly important. It holds up everything in that foot. So if you were going to take a scalpel to the bottom of your foot, you’d get the skin, and your next anatomical structure would be the ligament.
So it holds up all the different layers of the foot, which is very deep people don’t realize how deep the foot is. You have four layers of muscle, tendons, and then the most top part of the foot, that’s where all the bones rest on. So it takes everything into account.
Dr. Eric Chehab:
Explain what life is like for someone who develops plantar fasciitis. What are some of the common problems that they’ll have?
Dr. Carla Gamez:
They will present with swelling, pain. At first it’s pain just in the morning. Pain after certain exercises, pain coming from inactivity positions to active positions.
And it starts out as being very infrequent and all of a sudden, unfortunately, that condition progresses, it becomes constant. Every step that person takes it is painful. And if it’s really bad, you’ll actually see the swelling on what is the arch and heel portion of your foot, on the inside of that foot structure.
It really is painful because when we stand, when we walk, the first contact to the floor is that heel bone. And if you’ve never experienced that, I hope people don’t. But if you have, which I have also, it is excruciating pain.
Dr. Eric Chehab:
Now, your story of plantar fasciitis is very interesting. Do you mind sharing that?
Dr. Carla Gamez:
Of course. I had twins in 2003. Put some weight because of the pregnancy. And with that, my feet were really, really swollen. And with that, the ligament stretched out. I didn’t really know this because you’re in autopilot with twins, trying to still go back to work afterwards.
And as the twins were starting to become mobile around age two, I then also started become more mobile. And little by little, that pain was just constantly there. And I would try everything. I mean, I did the whole gamut. I even tried alternative medicine and it took two years to finally take that pain away.
Do I still get it? Yes, it can still come back. It’s never as intense as it was, but I’m still able to play tennis. I’m still able to run. I’m still able to be active. But I’m always managing the diagnosis and that stirred up my attention to this diagnosis, and I really started looking into it, and I started treating a lot of people with this because I’ve been there, and I know what it takes to get out of that painful cycle.
Dr. Eric Chehab:
What are some of the leading theories about why plantar fasciitis develops?
Dr. Carla Gamez:
It can be acute and chronic. And in the acute stage, it can be traumatic. You can actually fully rupture that ligament. And it’s usually on cutting type of sports, where it gets torn and if your foot swivels or turns abruptly and it’s already really tight to begin with, it just pops.
More of a chronic issue is, where it just starts to tear microscopically, and your body then wants to take care of it, and you have scar tissue, have inflammation on that area, and it will just be debilitating. But when I see it as a chronic situation, it’s not always swollen like it is when it’s acute.
A lot of times, people don’t realize it’s truly connected to some of the tendons that attach to that heel bone. And one in particular is the Achilles tendon and tight calves coming in from the muscle bellies of your calf. If those anatomical parts are tight. That plays into the position of that heel when it strikes the ground.
If it’s a cause from a tendon called the posterior tibialis tendon, which is. Coming in from the inside of your calf and coming all the way through the ankle and attaching to the inside of your foot, but on the arch area, if that’s weak, then your heel will be swiveled too much to the outside.
And that’s something we call pronation. We all have that pronation range of motion. But if it’s excessive, then unfortunately as that foot torques to the outside, then it’s an extra strain on that ligament.
There’s a lot of different factors to come up with a diagnosis. I think that’s why it’s difficult to put it into a cookie cutter recipe because there’s a lot of reasons why people present with this diagnosis.
Dr. Eric Chehab:
Just to review a little bit, some of the causes of plantar fasciitis, one is traumatic, doing a cutting sport, overload the ligament, the ligament gives. And we see that in other areas of the body, and there’s no reason why we wouldn’t see that in a ligament in the foot.
And then some of the chronic issues that can happen with plantar fasciitis, or this repair mechanism that is consistently going on throughout the body, but here in the plantar fascia, if that repair mechanism gets a little disordered or it gets a little exuberant, you can start forming scar tissue, chronic inflammation, pain in that area that can be exacerbated, even caused by some of the tendons that position the heel bone in a different position than you would ideally like. Is that about right?
Dr. Carla Gamez:
That is. I’m also going to add another population that presents this diagnosis are the weekend warriors. And it’s my middle-aged patients, and middle-aged nowadays seems to go from 40 to 60. The weekend warriors don’t really stretch or strengthen their lower extremity accordingly. I see a lot of people with weak core, weak hips and everything trickles down to that heel to that foot.
So if you have weak hips, or a weak core, or weak calves, or hamstring, and weak knees, that’s going to also alter and put strain on this ligament that’s only supposed to support your entire foot. I have to look at it, not just the heel, I look at the entire lower extremity.
I do a gait analysis, if they can, if they’re not limping. And I look at the position of their hips. I look at the position of their knees, and then I look at the position of that heel. And that heel dictates how that foot’s going to go. So if the heel strikes the ground, not ideally, everything seems to trickle down.
As well as, you know, no physician really wants to tell their patients, “Hey, you know what? You’re overweight. This weight is too much on that heel.” That plays into it too. Because as that happens, the bones in the arch of your foot will then be altered, there’ll become arthritic, and they collapse.
We’re supposed to be born with those bones in the foot in an arch form. And that will allow for a nice propulsion from heel to toe. However, when the little bones in your arch and your foot are so arthritic, they will lose their form and their positioning and their joints, and those bones will fall to the ground.
When that happens, that also puts strain on that ligament.
Dr. Eric Chehab:
Right.
Dr. Carla Gamez:
So all of that goes into why people present with the tearing or the chronic inflammation of that heel. So, the majority of my people are middle-aged, but I do get a lot of my older patients 65 and up that want to all of a sudden start exercising and are not conditioned very well and things starts to fall apart. And you have to tell them, unfortunately, they’re not 20 years old again. But it’s a condition that can be managed very well.
It can be self-limiting. If you don’t do anything, it can take up to two years. But I want patients to understand that when I’m done treating this diagnosis and they’re back to, for the most part, their activities, they can never leave this diagnosis. In the aspect that you need to always stretch out, and your lower extremity legs and calves and feet, You have to always strengthen them.
It’s just like brushing your teeth. What happens if you don’t brush your teeth? You get cavities. What happens if you don’t stretch your calves and stretch your tendons? You’re going to start to pull something. So I try to kind of relate that –
Dr. Eric Chehab:
That’s a great analogy with the brushing the teeth. It’s so true. Develop these habits of keeping our core strong and keeping our foot and ankle flexible and everything that leads to the foot and ankle, keeping it strong and flexible.
And so when a patient presents with plantar fasciitis. What are the typical symptoms? You mentioned pain in the morning, pain when they step that can be progressive. Any other signs or symptoms of plantar fasciitis?
Dr. Carla Gamez:
People can also present with pain on the outside of the foot. And that is two things. Basically they’re compensating and they’re swiveling their foot without even knowing it. And they’re effecting the tendons and the bones on the outside of the foot and they become painful.
As well as, going back to the anatomical part of that ligament, I said in the beginning, it starts at that heel bone, but the origin of that ligament starts out as one and then it branches off into three branches into the arch of the foot, and then it all comes in together and it reattaches at the ball of the foot.
Anatomically, we call it the metatarsal phalangeal joints. So the outside ligament can also get stretched out, and it can also cause pain. You can also, if the pain progresses and it’s really chronic, you can actually get stress fractures of the heel. And people don’t realize that at least 5%-8% of all these cases, there is stress fractures. And that’s why we always take x-rays on the initial visits, as well as if they’re not getting better with traditional treatments, then I’ll get an MRI. And then the MRI usually will tell me there’s a stress fracture or a bone contusion. And a bone contusion is bone bruise.
And a bone bruise is different than a bruise on the skin and it can linger and it can feel like you broke your foot. And then with that, also people come in and see these x-rays that have heel spurs, which are calcium deposits. And people will come and say, “oh, it’s the heel spur,” and I tell them, well, the heel spur tells me that it is how long you’ve been straining that ligament.
And you’ve been stranding that ligament asymptomatically, but all of a sudden it takes one turn or one adjustment to your shoe or anything like that. That can start the process of you feeling the pain and becoming symptomatic.
Dr. Eric Chehab:
Now earlier you mentioned the gamut of treatment for plantar fasciitis. So let’s go through that gamut and let’s start first with the non-invasive treatments for plantar fasciitis.
Dr. Carla Gamez:
90% of all these cases really do get better through conservative approaches. And that’s the first and foremost, I tell that to my patients.
And my approach is, we’re going to reduce weight-bearing, high impact activities. I’m going to have the patients already start a home exercise program for not only stretching your heel, your arch, but also targeting your Achilles tendons, and your calf muscles. As well as that, I really believe in physical therapy for this condition.
I send my patients to physical therapy, not to do exercises. I’ve already given them a home exercise program. But I’m sending them to physical therapy for basically a lot of deep tissue massage, a lot of techniques that they’re trained on to really loosen up that ligament, try to disperse that inflammation in that arch and heel, as well as the calf and the Achilles. And they’ll use tools, or there are techniques called Graston and ART, and I will be honest, at first they’re not very comfortable, but really, it’s all very effective.
And you look at the tennis shoes or the shoes they wear. So, I come in, I say, okay, you might need custom made orthotics, but at least let me start you out with a good over the counter orthotic that’s going to provide a good arch support. Because that’s going to help you walk better and it’s going to help you put your position of your heel in a more corrected position.
With that, also I instruct them, they may need to tape their foot. And what do I mean by taping of their foot? I mean, that certain taping techniques can hold that ligament in a correct position. And if that ligament is too stretched out and it becomes a lot more mobile than it should be, the taping provides a reinforcement of that ligament and then will allow that heel to not strain it as much.
Cortisone shots is also an option. I do a lot of them, but I don’t always offer that on that first initial visit. I tell my patients, cortisone is great, however, it’s a bandaid. And people want to come in and just get that done and be done with it. And they don’t want to put in all the hard work that goes into this. And I said, I’m offering you a cortisone shot only if it’s really swollen. It will provide a lot of relief, but it’s not the only thing I want you to do. Or if you’ve hit a plateau, I’ll give it to them. And they’ll be able to get a little further in the therapy, they’ll be able to get a little stronger in their other tendons.
I don’t like giving multiple steroid shots. I just don’t. There’s a downside to them too.
Dr. Eric Chehab:
Is there a risk of rupturing the ligament with repetitive cortisone shots?
Dr. Carla Gamez:
Yes. Typically, we say we only like to do a couple, two to three a year. I say the same thing with the plantar fascia, or any other, ligamentous injuries.
I really stick to two. And if those two, I don’t do them repetitively as well. I space it out because there is data out there and I’ve seen it in my own practice. So, I am wary of that, but there’s a place for a cortisone shot.
Dr. Eric Chehab:
Do you also use night splints? Is that something you use?
Dr. Carla Gamez:
Yes, I do.
Dr. Eric Chehab:
And do use those early on, or if people are having trouble– and are they comfortable to sleep in? I used a night splint, and I didn’t find it that comfortable, but in the end I still used it because I was so uncomfortable from the plantar fasciitis.
Dr. Carla Gamez:
I do believe in night splints, and I do recommend it, but I recommend it if the patient presents to my clinic with a lot of pain when they get up out of bed. And that pain is prolonged, and it just doesn’t get better after two minutes of walking around and loosening things up. I will recommend that night splint. And I will tell them this is temporary. And if you can’t do it every night, at least do it every couple nights, you know? I used it myself. It’s really uncomfortable, but it does do the job. But you find a lot of my patients, me included, at two in the morning will rip that night splint out and it’s it’s and if you do it too tight, you can get numbness in the ball of your foot. But it serves a purpose.
Dr. Eric Chehab:
I’m saying nightspots like, everyone knows what it is. What is a night splint?
Dr. Carla Gamez:
A night splint is a plastic brace that goes on the bottom of your foot and then goes behind your calf. And then it has Velcro straps to adjust the flection of your foot towards your ankle.
And the purpose for that is it will provide a stretch. And that stretch is able to be applied to not only that plantar fascial ligament, but also your calf and your Achilles. By the time you wake up, it will be stretched out, so when you get out of bed and you strike that ground at that first point where you’re going to do your morning routine, it’s not going to immediately be so tight or taut that it’s going to again, tear. Cause that’s exactly what happens in chronic plantar fasciitis.
Dr. Eric Chehab:
It’s those chronic micro-tears that you were referring to earlier
Dr. Carla Gamez:
Correct.
Dr. Eric Chehab:
That’s why it’s so painful with those first initial steps in the morning, because it’s been tight and the night splints will help keep it stretched out overnight so that when you do take that first step, it’s like it’s already sort of prepared for it to some degree.
Dr. Carla Gamez:
Correct. And, going on the night splint topic, the older the patient is that’s not going to really be tolerable. You do have splints that go on top of the foot too, that are less bulky and I’ll recommend that. And in case that doesn’t work out or the patient can not find the comfort zone and that type of a brace, then I’ll tell the patient, keep a towel or a band right by your bed.
And when you wake up, take 20 to 30 seconds per foot because whatever I recommend on one foot, you better do it on the other. So take that towel, wrap it around your arch of your foot, stretch and pull that towel so that you’re mimicking that same, stretch and pull from that brace and just hold it for 20, 30 seconds on each foot. And at least that will provide some relief when you step on to the ground from your bed.
Dr. Eric Chehab:
So to summarize the non-invasive treatment measures we’ve talked about. Stretching for the plantar fascial ligament and for the calf. We’ve talked about physical therapy where manual massage techniques and therapeutic techniques such as Graston or Active Release Technique, the ART can be very helpful. We’ve talked a bit about cortisone injections being, not a first-line of treatment, but something that can be helpful if someone’s very swollen or having a lot of pain or hasn’t responded to initial treatments. We’ve talked about the use of night splints to help our sleep be a source of stretching of the plantar fascial ligament and of the Achilles and calf muscles. And then, what other treatment options, you know, there must be some interests, particularly with plantar fasciitis for PRP injections and for maybe even stem cells. What’s your take on that?
Dr. Carla Gamez:
I definitely provide that. But the only thing I’m going to just back up on that, also orthotics and in the orthotics, I also like to get a gait analysis. In my visit, I’ll do a quick gait analysis. However, if I want really to see how their lower extremities are functioning, I will send them to physical therapy, where they will do more of a video gait analysis and I’ll get the results and I’ll go over their gait analysis with their patients. And then if their gait pattern is perpetuating the plantar fasciitis, then I will recommend custom made orthotics.
If that’s still all of that doesn’t work out, then it will go into alternative treatments.
Dr. Eric Chehab:
So the things like PRP and stem cells? I don’t do any stem cell injections. I don’t know if you’re doing stem cells. The platelet rich plasma injections, I do much more commonly. Okay. And what are the studies showing about platelet rich plasma for the treatment of plantar fasciitis?
Dr. Carla Gamez:
It’s mixed, but I will have to tell you, I don’t know if there’s really good research papers as far as this is concerned, with plantar fasciitis. It is mixed, and it’s been mixed for the last 20 years, but in my practice, I get 80 to 90% relief when I do the PRP injections. And I don’t know if it’s because after I present it, and after I do a PRP injection, I offload that patient. I mean, they’re not walking on that heel for one week to 10 days. Then they’re still in the immobilizer boot for another two weeks. And then we start passive range of motion.
I will tell you for the most part it’s pretty successful, but again, by the time the patient gets to that point, it’s that 10% going back to that population, and anywhere between 5 to 7 million patients are diagnosed yearly with this.
So you take that 10%, you know, it’s a lot of people. And this is 40% of my practice.
Dr. Eric Chehab:
Yeah. Okay. What are some of the invasive treatments for plantar fasciitis? Can you describe those?
Dr. Carla Gamez:
Yes. Open plantar fasciotomies. And what’s really more common these days are, it’s still a fasciotomy, but using, newer instrumental techniques . I don’t want to really say minimal invasive, but it’s almost like doing a little mini scope where you have a little stab incision at, I don’t know, maybe, a few millimeters and you’re going in with a cutting device and you’re just threading a little bit of that ligament.
Dr. Eric Chehab:
Can you explain to the listener what a plantar fasciotomy is?
Dr. Carla Gamez:
Traditionally, that plantar fasciotomy is done on the inside of that heel. And traditionally that incision is, two to three centimeters. And it’s done at a oblique angle inside of that arch. I, to be honest, I stopped doing them 15 years ago.
Dr. Eric Chehab:
Why?
Dr. Carla Gamez:
For two reasons: there is a high rate of post-op infection because of wound dehiscence.
Wound dehiscence is where the surgical incision splits open. And because where you’re placing that incision, you step on that ground, you step on that floor if those stitches pop open, that wound will pop open. And then there’s a high risk of infection to the surgical area.
And people used to also go in and shave that bone spur, which would also create inflammation. Or the surgeon goes in, and you cut almost the entire ligament itself, which I am so opposed because it is so important, in my view, of maintaining foot structure. You take that away? You get chronically hammertoes, bunions, you’re cutting, some of the tendons too– if you go too deep, you can injure the nerve in that area as well.
So I personally stopped doing them, but the minimal incision technique, I think there’s a lot out there that’s promising. I am trained in it. I really leave that one honestly, for the last resort.
Dr. Eric Chehab:
Okay. And then what about some of the high intensity ultrasound treatments, that aren’t tolerated in the office, but might require an anesthetic
Dr. Carla Gamez:
Shockwave?
Dr. Eric Chehab:
Yes.
Dr. Carla Gamez:
I’ll tell you honestly, I had to do shockwave. I got to that point and my experience, I did the shockwave, and that’s what really put me over that like allowed me to live my life and– recover
And I used to do a lot of shock waves, probably 10 years after that. But unfortunately, the insurance companies stopped paying for that surgery.
So people didn’t want to, and I could understand that, you know, because it’s not–
Dr. Eric Chehab:
You’re paying for the operating room costs and the anesthesiologists and your time, I mean, it’s just adds up very quickly.
Dr. Carla Gamez:
And whereas the PRP, which I do a lot. We can do that in the office.
Dr. Eric Chehab:
And again, we’re using this treatment for the 10% of patients who don’t respond to the noninvasive treatment measures.
The majority of patients respond to the non-invasive measures that you had outlined previously. And again, I want to re-emphasize the orthotics that I forgotten, I’m sorry about that.
So look, I think plantar fasciitis is a very difficult condition to live with. It’s a difficult condition to treat, in some regards because we don’t have that magic bullet that gets rid of it. But if I can summarize a little bit, it sounds like there’s a progression of treatment that will help almost everybody recover nearly fully, at least to the point where they won’t care about the difference, maybe? As long as they keep up with their home exercises and brush their teeth, so to speak on the plantar fascia side of things.
And, and then for that 10% of patients, we also have treatment for them. And some of this treatment has come into vogue and come out of vogue, but there are reasonably good treatments with predictable outcomes for that 10% of patients who can’t get better with non-invasive measures.
Dr. Carla Gamez:
Correct. I will also just add to this, the psyche to the patients that present with more of a chronic situation.
And I tell my patients, you need to be patient with this process. I can’t just give you a pill and it’s going to go away. And if I can have that patient understand–
Dr. Eric Chehab:
If you could, by the way, you’d be in the Bahamas–
Dr. Carla Gamez:
Oh my God, (laughs) without a doubt!
Dr. Eric Chehab:
So what do you tell that patient?
I tell that patient, I’ll be with you in that whole trajectory of the treatment and getting you back to at least if not a hundred percent of your activity, I will aim to get you back to 80% of that activity level that you so desire, but you have to just let me try to guide you and push you a little bit to get to that point.
Well, my guest today is Dr. Carla Gamez from Illinois Bone and Joint. Carla, thank you so much for being here and shedding light on plantar fasciitis. I totally appreciate your insights and thank you for being here.
Dr. Carla Gamez:
It was my pleasure. Thank you, Eric.
Don't Miss an Episode
Subscribe to our monthly patient newsletter to get notification of new podcast episodes.

