Osteoporosis
Osteoporosis is a skeletal disorder, characterized by low bone mass, that causes a structural deterioration of the bone. The resulting low bone mass and low bone quality increases the risk of a fractures–even in cases where patients report no or minimal traumatic events leading up to the break. Osteoporosis is often left undiagnosed until patients present with a fracture because it is an asymptomatic disease. Learn more about who is at risk, other ways to diagnose it, and what can be done to manage and maintain bone mass.
Hosted by Eric Chehab, MD
Episode Transcript
Episode 11 - Osteoporosis
Dr. Eric Chehab: Welcome to the IBJI OrthoInform, where we talk all things orthopedics, to help you move better, live better. I'm your host, Dr. Eric Chehab. With Ortho Inform, our goal is to provide you with an in-depth resource about common orthopedic conditions that we treat every day. Today, it's my pleasure to welcome Dr. Alejandra Rodriguez-Paez. Dr. Rodriguez hails from Colombia, where she graduated at the top, number one in her medical school class from the Universidad Nacional de Colombia Bogota in 2002. She moved to Miami, where she did fellowship and research training at the University of Miami School of Medicine, investigating the mechanisms and treatment of progressive damage after traumatic brain injury. She then went on to Philadelphia where she completed her internal medicine residency at the Albert Einstein Medical Center. She remained at Albert Einstein to complete her fellowship training in 2009 in rheumatology.
After fellowship, she practiced rheumatology in both an urban setting in Philadelphia and private practice and also in rural Indiana. Dr. Rodriguez has been with Illinois Bone and Joint Institute since 2015, and has treated thousands of patients with rheumatologic conditions. We are here today to discuss osteoporosis, which is of particular interest to Dr. Rodriguez. Alejandra, welcome to OrthoInform. And thank you for being here today.
Dr. Alejandra Rodriguez: Thank you for having me today.
Dr. Eric Chehab: So let's get right into it. What is osteoporosis?
Dr. Alejandra Rodriguez: So osteoporosis is a skeletal disorder that is characterized by low bone mass that causes a structural deterioration of the bone that increases the risk of a fracture in the patient.
They have low bone mass and low bone quality. So that's why the bone breaks.
Dr. Eric Chehab: So how has it defined? How do we know when someone has osteoporosis?
Dr. Alejandra Rodriguez: Sometimes the patient presents with a fracture, with a fragility fracture. So what is a fragility fracture? A fracture that happens with minimal trauma or when they have just a simple fall from standing.
Sometimes patients can fracture without doing anything in particular, especially in the spine. They can cough, they can sneeze or pick up something light and they can have a fragility fracture. So a lot of times, the patients aren't diagnosed through the symptom because osteoporosis is an asymptomatic disease.
So the symptom of it is having a fracture. The other way, how we diagnose this disorder is through a test called a DEXA scan. And that it's usually done as a screening test in patients that are in general older than 65 that have no risk factors or sometimes they're done younger when they have different risk factors that we know puts them at risk for osteoporosis.
Dr. Eric Chehab: It sounds like osteoporosis is something that we know we have the hard way, by developing a fragility fracture or with something we can screen for. And obviously the role of screening would be for prevention. How do you approach a patient who you think may have osteoporosis?
Is it something that inevitably develops in every patient or is it just in a select few?
Dr. Alejandra Rodriguez: Usually osteoporosis happens more commonly in women, and men is actually very underdiagnosed because of that reason. So I think that primary cares are more in tune to screen for osteoporosis in women. We know that white women, uh, have a higher risk. We know Asian women also have high risk. We know that men just by biophysics, they have thicker bones and the risk of having osteoporosis is less. We know that women that have thin frame also have high-risk. It is important also to take a note of other risk factors, medications, a lot of medications increase the risk of osteoporosis, especially medications that we use in our rheumatological patients like steroids.
And a lot of people have heard that. They decrease the bone mass by different mechanisms. Other medications that are commonly used are the proton pump inhibitors that are medications used for gastritis. Uh there's some of them are over the counter. So those also increase the risk of osteoporosis and low bone mass. Other things that happen in women when we may have menstrual disorders or they have a late onset of the menarche, which is a first menstrual period, or early menopause. Those hormonal changes also increase the risk of osteoporosis. Other diseases, um, multiple endocrinological disorders like hyperparathyroidism, hyperthyroidism, uh, sometimes diabetes, cancers of the blood also increase the risk, a lot of their rheumatological and auto immune disorders such as rheumatoid arthritis, lupus, not only by the medications that we give, but by the mechanism of the disease itself, they increase the risk. So I think that rheumatologists in general, we are more in tune diagnosing this disease prior to the fracture.
Dr. Eric Chehab: If I can summarize a little bit, osteoporosis is different in men and women, in terms of the incidence of it, it's different by ethnicity. It's affected by other conditions that patients may have, it can be affected by medications, some very common medications and all this can accelerate the development of osteoporosis in anybody.
Correct. Let's start with gender differences. What's the difference between men and women besides the just more bone mass to begin with. Don't both men and women lose bone through the lifetime. And when does that start?
Dr. Alejandra Rodriguez: Yeah, so usually, uh, normally, for all humans, we reach our peak bone mass at the age of late twenties to early thirties.
So we call that a peak bone mass. And then as we age, usually around the late forties, we start losing bone and normally. So in women, estrogen is a very important factor in that equation. The hormonal differences are significant, but there are other mechanisms in the changes of bone quality that affect men as well.
So that's why I think it's underdiagnosed. I think in general, we're not in tune with that. And then just the composition of the bone. The physics of the bone of a man, they have bigger bones in general. So they're not as fragile as a woman has a thinner bones in general, or the frame is different.
Dr. Eric Chehab: Right. We learned about that also that when people age, the frame changes a little bit, it tends to get a little bit farther away from the the center of mass and that has some resistance to the loss of bone density. And so those changes in the shape of the bone are actually somewhat beneficial and somewhat compensatory for when we're losing bone mass.
But men start with a bone that's farther away from that center of mass. And so they have more sturdy bone, even if they were to lose more bone to begin with. Correct. So let's go right into it. You mentioned that it's an asymptomatic disease, so people who are developing osteoporosis don't know they have it. Correct?
Dr. Alejandra Rodriguez: Correct. So I tell a lot of my patients because they come in and say, I don't feel anything, why do I need to take this medication? So we know that osteoporosis is very common. So we know that one in two women and one in four men over the age of 50, they have a high risk of having a fracture.
We know that it's a very costly disease. So the treatment of osteoporosis, we know by the year 2018 was about 52 billion, in the United States, just by the cost of hospitalization, fracture care. So on and so forth. It is also deadly. We know that a patient that has a hip fracture has about a 25% to 30 percent of dying in the first year after fracture. We know that about 25% of those patients also go to long-term care facilities. They never recuperate their baseline function. In up to 50%, they lose their independence.
The woman's risk for fracture is a combined risk of having uterine breast and ovarian cancer. And for men they're more likely to have a fracture than having prostate cancer. So it's a very common disease.
Dr. Eric Chehab: We have a saying in orthopedics because we treat so many of these hip fractures that we enter the world through the pelvis and leave the world through the hip.
And the hip fractures are underappreciated, deadly fracture and, you know, people think of it as all. It's just a broken bone, but it's, it's so much more than that. And it frequently spells the beginning of the end for many people when they fracture a hip.
Dr. Alejandra Rodriguez: Correct. You're totally right.
Dr. Eric Chehab: Yeah. I did not know that about being that common in men and I have this absolute bias that it's so much more common in women. And I don't even view this as a huge problem in men, though I know it is. And it must be difficult to overcome that bias, particularly with male patients who you're telling you have osteoporosis, you need this treated.
Dr. Alejandra Rodriguez: Yes. Correct.
Dr. Eric Chehab: Now you mentioned DEXA scanning as a means of screening. Explain that to patients, what a DEXA scan is.
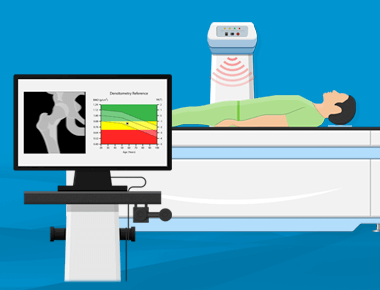
Dr. Alejandra Rodriguez: So the DEXA scan is a test that is done in a machine that you have to lay down is x-ray based. But the amount of radiation that you get with a DEXA is very minimal, is less than a cell phone probably or traveling in an airplane. So basically we scan the lumbar spine and the hip, most commonly, sometimes we scan the distal forearm, depending on different risks of the patients or circumstances also. And that gives us information regarding the bone density. So it's important to know that the bone strength has two components: the bone density and the bone quality.
Measuring this bone density through the DEXA scan can gives us information about the fragility of the bone or the risk of fracture.
So that is why it's a very important tool. And that's how the W.H.O. created these criteria to help us diagnose osteoporosis. So they created this thing called a T-score that is based on a standard deviation of the average bone density of healthy 30 year olds. And then if your, T score is more or equal to minus 1.0, your bone density is normal. If it is between minus 1.0 and minus 2.5 is what we call low bone mass or osteopenia as most people know it. And when it's below minus 2.5 is considered osteoporosis.
You're actually, when you have a DEXA scan, you're being compared to a group of 30-year-old women. Correct? And that's, that's the standard. So that's picked as normal bone density. And then if the minus one, is that a single standard deviation? In other words, you're sort of at the percentile of bone density when you're at minus one.
Yes. Correct. So it's one standard deviation from the average.
Dr. Eric Chehab: When you are at minus 2.5, you're at what percentage?
Probably like 5%, right? I mean, you're two standard deviations away from, so you're really in the fifth percentile of all women, age 30, for bone mass.
Dr. Alejandra Rodriguez: Correct. And the reason why it's compared to that population around age 30 is where we were mentioning before around age 30 or late twenties is when you reach your peak bone mass. So theoretically that's when you have your highest bone density.
Dr. Eric Chehab: So it's funny. I'm going to take a little sidebar. I had a mentor in residency training who was a metabolic bone specialist. So he had an osteoporosis practice and he talked about the standard being 30-year-old milkmaids in Wisconsin. And he often joked that if we only had the comparison against waif models in Los Angeles, that we'd all feel a heck of a lot better about our bones.
Dr. Alejandra Rodriguez: That is, that is a funny story. Definitely. Definitely. And actually nowadays, we're seeing more younger females having osteoporosis because I think they're probably not reaching their adequate peak bone mass with all these new diets going dairy free and all these new, um, you know, standards of beauty that a lot of younger females tend to have eating disorders, which is a major problem.
Then we're seeing that you're reaching a lowest peak bone mass. So obviously you start with less and as you reach menopause, then.
Dr. Eric Chehab: So you're alluding to this a bit. I mean, in order to prevent osteoporosis, there's a lot of work that can be done to increase your peak bone mass, so that when you actually start losing bone, you have a better starting point to lose that bone mass. Is that correct?
Dr. Alejandra Rodriguez: Definitely. So ideally, you should have a, an adequate intake of calcium and vitamin D. In general, we recommend that we diet at the most part. So in younger females, we recommended that they have their intake of dairy or dairy related products or that they have calcium. Supplements in younger age are not recommended necessarily because they there's no data suggesting that that decreases the risk of fracture when you're younger. When you have osteoporosis or risk factors or low bone mass, there is data suggesting that calcium supplements do decrease the risk of a fracture. There has been controversy regarding the supplements and the past few years, regarding increased risk of cardiovascular disease.
Unfortunately, there's a lot of studies that are showing positive and negative effects. So that's still up in the air. There's still a lot of controversy, but in general, we do recommend that. However, we know that the absorption of calcium is better through foods. So in general, I recommend my patients that, they should have about 50% with diet, 50% with supplements. And the reason being is that as you age, having a lot of dairy and things like that, it's difficult. Not only because as we age, also we develop lactose intolerance, most adults, but also because a lot of our patients have high cholesterol and other problems. And then they have to limit their intake of cheese or other fatty foods. And dairy has some fat in it. And also it's just difficult from the amount that we recommend. It should be in post-menopausal women and men over 50, about 1200 milligrams of calcium daily. With the vitamin D, it is recommended to have about 800 units to a thousand units, but that's very variable, especially here in Chicago.
We don't get much sun through the year or at least six months of the year. We don't get that. So we see a lot of vitamin D deficiency and a lot of patients might need higher than that. Vitamin d is not readily available in foods as much as calcium, so a lot of patients require supplements.
So we usually measure their level and we try to target to a normal level, and give them directions regarding how much they need to take.
Dr. Eric Chehab: So the diets obviously critically important to building bone mass when you're younger to reach your optimal. Peak bone mass, but it's also critical to maintenance of bone as you age, so that you're losing bone at a slower rate, correct?
Yes. Okay. What other factors besides diet can be helpful for patients maintaining their bone mass as we age?
Dr. Alejandra Rodriguez: Exercise is also very important. Okay. So types of exercise. So, yeah, so weight-bearing exercises are very important. We know that there are some impact exercises also like jumping, jumping jacks and other things like that, or exercises that focus more on your hip girdle area that contracted all the gluteus muscles. Those exercises increase your hip bone density and other weight-bearing exercises, like lifting weights and other things like that. They tend to help with your lumbar spine bone mineral density. So a lot of patients tell me, Oh yeah, I exercise. I walk.
So walking does not help in increasing their bone density in studies. However, we know that patients that are active have better bone density in general, or is good for your bone health, but also is good to decrease your risk of falling.
Dr. Eric Chehab: As you alluded to at the beginning, the whole purpose of the treatment of osteoporosis is to prevent fracture. Correct. A patient frequently doesn't know they have osteoporosis until it's too late, because it's a silent asymptomatic condition They've already broken.
Correct. If you have a patient who's exercising, and they're less likely to fall, because of better balance through the exercise, then they're obviously less likely to break because they're just not falling.
Dr. Alejandra Rodriguez: Correct. So that is very important. I also tell the patients to work on their core and balance training, especially as they age, to decrease the risk of falling.
And also we talked about different other things regarding fall risk. As you age, you have to make sure that you get an eye examination, that you have adequate glasses, uh, in older patients, I tell them not to have loose rocks around the house or try to prevent having decorations or things that they're going to trip on all over.
A lot of our patients go to the bathroom at night. And I do see them falling from the bed or just tripping at night. And I tell them to have an adequate lighting or like a nightlight in the path where you go to the bathroom so that they can see. And also have, um, modifications in their bathroom if they need, if they have weakness, if they need any sort of stool or any handle in their shower or by the toilet.
That's also very important just to reduce overall risk of fracture also. You know, with older patients, polypharmacy is a problem. So they take a little medication sometimes that can make them drowsy or dizzy. So that also we go through those lists and try to see what can be discontinued or minimized or used m ore sporadically if necessary.
Dr. Eric Chehab: The treatment of osteoporosis really has a lot of preventative strategies. It's preventing the loss of bone, preventing falls with all of these suggestions that you have for in the home, with the nightlight and getting up and making sure you're not going around when you're drowsy after medication.
So it's, it's really a preventative treatment because these fractures can be so devastating if they occur. Correct. Now, just to switch back a little bit, you mentioned earlier that a DEXA scan measures bone density, but there's also this concept of bone quality. Do we have any tool to measure bone quality?
Dr. Alejandra Rodriguez: Unfortunately, in clinical practice, we don't, but we know that even sometimes with treatments for osteoporosis and you have stable bone density numbers, we know from research that the bone quality continues to improve that the micro architecture of the bone improves with treatment overall, despite of the number of their bone density.
Dr. Eric Chehab: So we're kind of using bone density as a surrogate measure of bone quality. Correct. But there's still a subtle difference.
Dr. Alejandra Rodriguez: Yes. So both of them, those two components make the bone strength in general. So I try to explain to my patients, sometimes they see that their bone density is the same or continuous.
And why do we continue these medications? And I explained to them that that's the reason. And also we know that from studies, the stabilization of bone density means that the success of treatment also. So I also tell them that they should not expect that the medications make them go to normal bone density. That never happens really, or very rarely. So, that is a way we have to monitor and estimate the risk of fracture.
Dr. Eric Chehab: DEXA scanning is one tool for defining osteopenia and osteoporosis and bone density and bone quality. What are some other tools at your disposal that can help you determine what would be the best preventative treatment strategy for a patient?
Dr. Alejandra Rodriguez: So things that we do also in the evaluation, we check some blood tests, to evaluate if there's any other conditions that are related to the bone loss. We call secondary causes of osteoporosis or the beginning. We kind of see if the patient has any endocrine disorder or any other disorders that can weaken their bones further than just the regular osteoporosis.
Dr. Eric Chehab: What are the common endocrine disorders?
Dr. Alejandra Rodriguez: Thyroid. So we usually check vitamin D deficiency, that one that is very common. So we always check vitamin D with thyroid disorder. Kidney disorders also can cause bone loss. And parathyroid disorders, also disorders of phosphorus and magnesium.
There are rare genetic disorders that can cause us to process or other metabolic diseases. So we always kind of look for them.
Dr. Eric Chehab: So you screen for those things with blood testing–
Dr. Alejandra Rodriguez: Testing in the initial evaluation, and regarding prevention, I think everybody, qualifies for those suggestions that I mentioned, uh, regardless of their needs.
Dr. Eric Chehab: Sure. Is family history important?
Dr. Alejandra Rodriguez: Family history is very important. Good that you mentioned that. So if you have a family member that has had a fracture or has osteoporosis, especially a first degree relative. So that's something that we always ask the patients first degree relatives. Uh, mother, mum or dad, uh, if they have had a hip fracture that actually increases your risk of fracture significantly and that's part of FRAX.
Dr. Eric Chehab: So explain what FRAX is. I I'm, I'm sort of obsessed with FRAX. I, I use it frequently with patients who ask me questions about osteoporosis and as a surgeon, I frequently treat poorly managed osteoporosis that we end up operating on the broken bone and obviously we would be much better off preventing the bone from breaking in the first place.
And so I love the idea of FRAX. Can you explain what that is?
Dr. Alejandra Rodriguez: So FRAX is an algorithmic calculation.
Dr. Eric Chehab: What does it stand for? Fracture risk assessment tool, I believe, right?
Dr. Alejandra Rodriguez: Yes. Correct.
Dr. Eric Chehab: So explain what the fracture risk assessment tool is. I use it. Just to tell patients, look, there's more to this than just your T score. Um, your bone density tests from a DEXA scan, which is comparing you to 30-year-old women.
And obviously as we get older, you're not going to have the same bone density that you had when you're 30, because we all lose bone. So you wouldn't expect to be in the 90th percentile of 30-year-old women when you're 80 years old. So what is the fracture risk assessment tool? What does it tell us what are some of the variables that go into it?
Dr. Alejandra Rodriguez: This tool is an algorithmic calculation based on different risk factors of the patients. So it was created by a group looking into helping the clinician, um, as, as the risk of fracture in the population of patients that have low bone mass. So osteoporosis, we have clear-cut diagnostic criteria and triggers for treatment in patients that have a bone mineral density T-score of less than minus 2.5 or a patient that has a hip or avertable compression fracture.
Those patients automatically have osteoporosis and they require treatment. So that population between minus 1.0 minus, 2.5 low bone mass, I usually explain to my patient that does a gray zone. And FRAX helps us to determine the risk of fracture. So it takes into account age, their weight, different risk factors.
Some of them are, um, history of parental hip fracture. So either your mom or dad had a hip fracture, if you have had a fracture, a fragility fracture, also smoking, use of glucocorticoids. If they have history of rheumatoid arthritis, if they consume more than three alcoholic beverages a day, it also takes into account the T score.
Sometimes you can calculate it with them without the T score. And that gives you a number and usually they, um, In the criteria of treatment when they have a risk of major super-rich fracture, more than 20% that prompts you to suggest treatment to that patient. Or if you have a risk of hip fracture more than 3% based on FRAX calculation.
So I usually tell my patients, that helps me put them in, within that grace zone to see if they're closer to osteoporosis, if they require treatment or if we could continue to monitor them without a pharmacological treatment, obviously making all those changes regarding lifestyle, calcium, vitamin D, exercise.
So across the board, in all the patients that have some degree of low bone mass, those are indicated.
Dr. Eric Chehab: So the FRAX is a useful tool for those patients in the gray zone, who don't have fully defined osteoporosis with a T score greater than minus 2.5. Meaning like minus three, minus one. And, um, also for patients, who've had fractures, they are of the hip or of the wrist or of the spine.
So those are the fragility fractures that are osteoporosis defining. So there's this large swath of patients who are in this gray zone and the fracture risk assessment tool can help give you, it gives you an output of what your estimated risk of fracture is over the next 10 years, correct? Yes. Correct.
And so that risk of 3% or 5% of having one of these fractures over the next 10 years can help you make a decision, do we treat with diet, exercise, supplements, and nonpharmacologic treatments versus do we treat with a pharmacologic agent? Correct.
Dr. Alejandra Rodriguez: Also, um, well there's some caveats regarding FRAX.
So as I mentioned, it takes into account those risk factors of, of those. But for example, we know that definitely a patient that takes five milligrams of prednisone is different than a patient that takes 20 or 40. So it doesn't account for that dose change. Also a patient that smokes one to two cigarettes a day is different than someone that smokes two packs per day, or someone that has had five fractures.
You know, I have some patients that have fractured five vertebrae versus somebody that fractured a wrist.
Dr. Eric Chehab: So that's super interesting. It's, you know, I think of FRAX as a more refined tool for evaluating osteoporosis than just say a DEXA scan. Yet even the FRAX tool could be more refined because it doesn't take into account these factors of how much medication you're taking and whatnot.
Do you think there are these tools developing to help be more refined about–
Dr. Alejandra Rodriguez: Yeah, they're looking into different things to help us be more precise in the treatment of osteoporosis, but also that clinical judgment is still comes into play. So we get the FRAX score. And, you know, if we know that the patient has other risk factors or, we take into account other things that are mostly clinical gestalt kind of situation, then you might, even though they don't meet the trigger for the FRAX score more than 20% or 3%, we might start them on treatment.
So I usually try to explain that to the patients because they say, Oh, So, and so was started on Prolia or so-and-so was started on this and, and that's how we made decisions based on their risk factors. So everybody's different. So that's why it's important to have an evaluation and talk to your doctor or seek a specialty evaluation so that that treatment can be tailored to you.
Dr. Eric Chehab: So let's get into some of those treatments, the pharmacologic treatments.
So we've discussed in some detail, the nonpharmacologic treatments for fractures. Let's talk about some of the pharmacologic treatments for osteoporosis, and preventing fractures. First of all, what are some of the common treatments that are available to patients?
Dr. Alejandra Rodriguez: So, um, the most common ones are bisphosphonates. We call them this. A group of medications that, um, inhibit a cell called the osteoclast. That is the one that eats up bone pretty much or helps with the bone resorption. So, um,
Dr. Eric Chehab: If you slow that bone resorption, you're going to have more bone leftover.
Dr. Alejandra Rodriguez: And the cells that build that bone, which are the osteoblasts can build that bone. Fosamax is one that is probably people know it most commonly. There's some oral, so Fosamax is one. Then we have Actonel, Boniva and there's some IV. Boniva can be IV or Reclast, which is a yearly formulation.
So those are the bisphosphonates. Those are the most common ones. There's other treatments that are parenteral, so meaning they are subcutaneous or mostly subcutaneous. Really. Prolia is another one that is very commonly known. There's two more that are what we call anabolic. And what that means is they stimulate the osteoblasts because they're hormones that are recombinant and similar to the parathyroid hormone.
That is a natural hormone that, uh, leads, um, bone formation.
Dr. Eric Chehab: So the two classes are one set of medications that can inhibit the cells that take away bone. Correct. And so therefore leave more bone behind. And then there are the other class of medications that build bone by stimulating the cells that make bone. Correct.
Many people don't know this, but. But bone is a metabolic organ. It's constantly in turnover. And these cells sort of work in a continuous dance where some cells are taking away bone. Other cells are putting down bone. And so if you can slow down the ones that are taking away bone or speed up the ones that are making bone, you can help build at least more bone density.
Maybe better bone quality or definitely better bone quality.
Dr. Alejandra Rodriguez: Definitely. So they work in both. So they help with the micro architecture of the bone and increasing their bone strength in those trabecula indefinitely.
Dr. Eric Chehab: Why would anybody be resistant to taking these medicines? I mean, it sounds like a home run.
Dr. Alejandra Rodriguez: So in the year, two thousands around that. time, there was a lot of press regarding two very rare side effects of this medication. Well, one is called osteonecrosis of the jaw and the other one is a typical femoral fractures. So the thing is that back then, um, patients were left on these drugs for ages for 10 years, 15 years.
So when those studies started to come up and I started to notice the relationship between the drugs and there's rare and devastating side effects, then there was a significant decline in the diagnosis and then the treatment of osteoporosis between the year, like 2005, 2012, according to some studies, there was a steep decline in the use of these medications because patients got very afraid and providers as well.
So let's talk about osteonecrosis of the jaw. So a lot of patients have this misconception that they're going to take these medications and they're going to have jaw pain, or they're going to have teeth problems or things like that. So I try to explain that that's not the case. Osteonecrosis of the jaw is a non-healing ulcer in the maxillofacial area in patients that require intensive, uh, dental work like implants mostly.
Teeth cleaning is not going to affect you or having a root canal even necessarily. Those ulcers, they heal, usually the patients that are high-risk are the ones that take high doses of bisphosphonates that sometimes it's used in cancer treatment or patients that are debilitated or that are on chemotherapy.
So those are the most common patients that develop this, um, very rare condition. So the absolute risk of having that in a patient taking bisphosphonates, it is less than 0.001%. So is extremely rare. The other rare side effect is the atypical femoral fracture. So patients say, why am I going to take a drug? That is going to put me at risk for fracturing if I don't want a fracture to begin with. So these are different fractures. So a hip fracture is usually intertrochanteric. Or in the femoral neck, these are what we call subtrochanteric fracture. So they, they have been more in the, in the shaft of the bone and we know that their risk of having this rare side effect, again, happens with prolonged use of bisphosphonates or the medications from osteoporosis because these two rare side effects are described across the board with all the medications.
Dr. Eric Chehab: So the more you take for a longer period of time, the greater the risk of this still very, very rare problem of osteonecrosis of the jaw or an atypical femur fracture, which is not a typical fracture that we're preventing around the hip, which is very close to the joint, but a fracture that's farther away from the joint and down the leg.
Dr. Alejandra Rodriguez: Correct.
So usually, the patients have what we call symptoms of it with an osteoporosis fracture. You don't have any symptoms. It happens and that's it. So the patients can have a thigh pain, lateral thigh pain. And then, you can see some early changes before a fracture. You can see thickening of the cortices of the shaft–
Dr. Eric Chehab: Cortical beaking that we see on some X-rays.
Right. Exactly. So you can have these early signs, so it kind of develops with time and we know that early on, you have the incidence of it is like around 0.01% at three years of use of bisphosphonates, more than eight years is 0.1%. So it does increase. We know that around eight to 10 years of use is when there is an elevation of the risk, but still is, is very low.
It's one in 10,000, the 100,001 in 10,000. I mean, very, very low risk. Um, you're probably at a higher risk of fracturing your femur driving to the pharmacy to pick up your medicine than taking the medicine, correct?
Dr. Alejandra Rodriguez: Correct. Okay. So I usually, that's why when these drugs and also we know they linger in the bone.
So that's the theory behind drug holidays. So that's, after all this reports started, we started doing that. And it's because we know that around that time you start having higher risk of this, uh, typical side effects. So we give a break, uh, of these medications and there are studies suggesting that, being off Alendronate or Risedronate or risedronic acid for about three years, you still have a significant decrease in fracture risk, despite of the fact that you're not actually taking the medication. So we do that very commonly now. So that's why I think we even see less of this, because a lot of physicians are now more in tune on that in the past, they used to be like, Oh, take your Fosamax.
And it was like taking a multivitamin. Now that doesn't happen.
Dr. Eric Chehab: The bisphosphonate medications, Fosamax, Alendronate, that are oral medications inhibit the cells that resorb bone, and there are other medications that you can use. Prolia is one of them, correct? Correct.
Dr. Alejandra Rodriguez: So Prolia is another anti-resorptive, but it acts in different pathways.
It is given every six months, it's a really good medication, but there is an important caveat with this medication compared to the bisphosphonates. It does have as slightly lower risk of having the atypical femoral fractures and ONJ versus bisphosphonates, but we know it doesn't linger in the bone, as I was saying with the bisphosphonate.
So there is some misconception that will across the board with medications, for us to process, you have to do a holiday. This is only applicable to the bisphosphonate category. We know that with Prolia and especially through their pandemic, we've seen a lot of these cases, because the patients obviously early on, they didn't want to come to the office, they miss their doses.
So that was a major problem. And it is because we know that with Prolia. If you don't give it within one to three months after you're due for your dose, you'll start having a rapid bone loss, uh, and you can have increased risk of vertebral fractures and multiple vertebral fractures. So unfortunately I have seen several patients with these problems, especially this year through their pandemic.
We do know that fortunately, if they go back on the regimen, we kind of slowly build up again, but it is important to know that with Prolia, there is no holiday to be given. It is a medication that at this time is recommended to give long-term. And if there is any reason to discontinue it, it should be followed by an antiresorptive agent, bisphosphonate, for a period of time to prevent that rapid bone loss.
Also mentioned in other medications, the anabolic medications, uh, surely there are medications that are given only for a short period of time for about two years. Those are team TYMLOS and Forteo. And also those medications, I tell patients are like a boost for your bone density because they're are stimulating those cells that build that bone.
And after that cycle is completed, ideally, you should be an anti-resorptive. So it's not just to be given one time and that's it. So it's important to take that into account.
Dr. Eric Chehab: We've obviously learned a lot from using the medications. And now do you think we're in a pretty good spot with preventing these fractures? Are there, is there more work for us to do medically, what's the biggest hurdle of preventing these osteoporotic fractures that can have such devastating consequences?
Dr. Alejandra Rodriguez: So I think that at this time we're doing a better job of prevention with, I think people overall are more in tune with diet, exercise, being healthy, eating healthier. So in that sense, I think, uh, we come a great deal, but. Regarding, uh, diagnosis and treatment of osteoporosis, actually, unfortunately, we continue to see a decline in diagnosis, a decline in treatment.
And also another hurdle that we have to jump is the lack of reimbursement for DEXA scanning. And especially with the pandemic, you know, a lot of businesses went down and everything. And if something is not financially feasible, it's difficult to continue it. So we do continue to see a lack of diagnosis, therefore, a lack of treatment.
Dr. Eric Chehab: Well, this seems like a classic, an ounce of prevention is worth a pound of cure. And osteoporosis treatment is absolutely this.
Dr. Alejandra Rodriguez: Definitely it's important. And at IBJI, we have a comprehensive program. We have a DEXA scan. We have a wonderful technician that is recognized worldwide. He's very knowledgeable.
We have an infusion center in which we give all the medications that are FDA approved for osteoporosis and our group of rheumatologists. We are experts in this condition as well. And also we have our orthopedic counterparts, um, that, um, are in tuned with osteoporosis
Dr. Eric Chehab: We're experts at treating the failed prevention of these fractures.
And so, you know, the Orthopedic Academy has recognized this for many years, that if we could become more skilled at preventing fractures, we'd be doing a much, much greater service than using our skills to fix these fractures. And they had a decade of Own the Bone, and I hope that was helpful in raising awareness of osteoporosis.
Dr. Alejandra Rodriguez: Yeah, definitely. And there's different hospital settings. There's these things called a fracture liaison programs. And I think here in IBJI, we're trying to do that as well. So that, that patient that has a fracture is recognized and is directed to have a DEXA scan and see a consultation with one of the rheumatologists or with their primary care for evaluation and further treatment.
Dr. Eric Chehab: So where are you most optimistic about the treatment of osteoporosis? Is it in the nonpharmacologic treatments. Is in the pharmacologic treatments, is it for both?
Dr. Alejandra Rodriguez: I think both arenas are important. I'm excited about newer treatments that are coming out, down the pipeline. Two years ago. There was a new agent that has dual action, uh, called Evenity and we're very excited about the approval.
Dr. Eric Chehab: So that works on both the inhibition and the growth of the bone.
Dr. Alejandra Rodriguez: Yes. So it has both actions. So we're excited about that medication. So there's a lot of newer things. Also in IBJI, we have a program called bone health program. So because we know how important it is, exercise. So we have a multi-disciplinary group of physical therapists, nutritionists, and this program encompasses health coaching, nutritional coaching, and physical therapy for the patients that have osteoporosis or that have had a fracture because also with the exercise prescription, I call it, everybody's different because someone that is 90 year old and has a fracture has a much different functional requirement than somebody that is 50 or 60.
Right. And also the capability of what kind of exercise you need to do. When I was talking earlier about impact exercises, you know, as an 90 year old cannot be doing jumping jacks. So, so our physical therapists are really good at tailoring that program to your needs. Um, also we have patients and I have several patients that are in their seventies or early eighties, and they still ski.
They still do a lot of things versus somebody that is more sedentary at home, or that has other conditions that impact their balance significantly. So evaluating all those things and tailoring a program to that person is very important. I'm excited about doing all that comprehensive treatment program that is multidisciplinary here at IBJI.
Dr. Eric Chehab: Our guest today is Dr. Alejandra Rodriguez-Paez.
Dr. Rodriguez, thank you so much for taking the time to be here.
Dr. Alejandra Rodriguez: Thank you. It's a pleasure talking to you today and hope everybody feels that this is helpful.
Don't Miss an Episode
Subscribe to our monthly patient newsletter to get notification of new podcast episodes.

