Searching for arthritis advice from a specialist? You’re in the right place! Sheela Metgud, MD, fellowship-trained rheumatologist with Illinois Bone & Joint Institute (IBJI), recently presented with the Arthritis Foundation at their “Live Yes! RA, A Personalized Goal-Setting Event.” We have her top takeaways from the presentation that will help you live with your rheumatoid arthritis (RA) this season!
First, a little background on auto-immune disease. Auto-immune diseases, such as rheumatoid arthritis, cause your body to attack its bones, joints and cartilage which can cause high inflammation, joint swelling and pain. Any joint can be affected. The most common are elbows, wrists, fingers, knees, ankles and toes.
Here are Dr. Metgud’s key takeaways on how RA may affect your health, tools to living with RA, and how to care for yourself with RA.
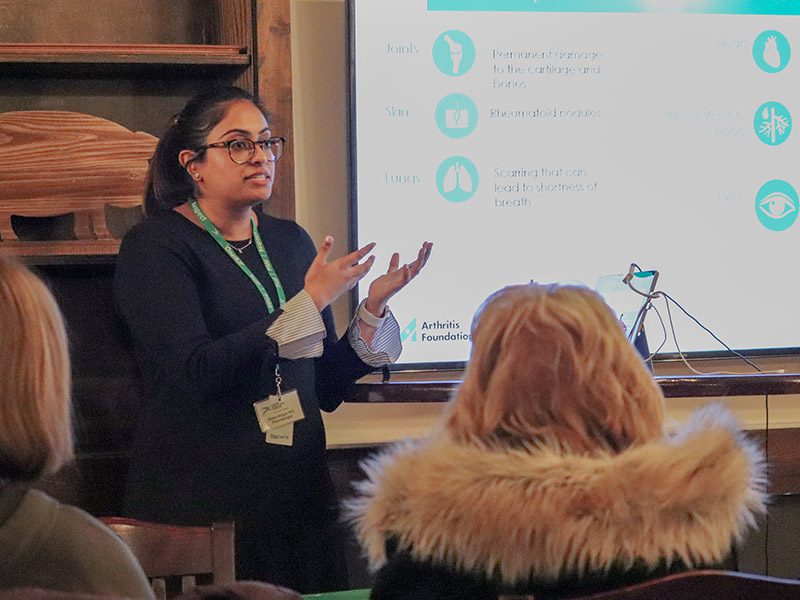
Dr. Sheela Metgud presenting at the Arthritis Foundation's Live Yes! RA event.
How RA may affect your health:
- Joints: Permanent damage to the cartilage and bones
- Skin: Rheumatoid nodules
- Lungs: Scarring that can lead to shortness of breath
- Heart: Increased risk of heart attack and stroke
- Blood and blood vessels: Can lead to damage in the nerves, skin, and organs and anemia
- Eyes: Dry eyes, inflammation, glaucoma and cataracts
Tools to help you live with RA:
- Health tracking tools: use health tracking to monitor RA and record symptoms regularly. Arthritis foundation offers a Better Living Toolkit online to help patients with this. Health tracking can be helpful for patients to monitor symptoms and notice patterns with regards to disease flares and triggers. Keeping track of your symptoms and disease self-management can help maintain a good quality of life.
- Goal setting: Personal and medical goals. Setting a SMART goal can be a useful tool to achieve these elements.
- Specific: Say exactly what you want to accomplish.
- Measurable: Have concrete steps to track progress.
- Attainable: You know it’s within reach.
- Relevant: Reaching the goal is meaningful to you.
- Timebound: You have an end date to work toward.
- Health care provider communication: Be upfront. Be completely honest. Be open. Be assertive. Establish good communication with your doctor and come to appointments prepared. You’re not alone when you connect with your health care team and your community. Share your success and progress and get involved with community arthritis programs!

How to care for yourself if you have RA:
- Regular physical activity. This includes low impact exercise, aerobics, strengthening and flexibility.
- Eat a nutritious diet. Eat foods rich in omega 3 fatty acids, vitamin C can help build cartilage and avoid processed foods. Read more about foods that can help arthritis.
- Use heat and cold therapies. Use this therapy for 20 minutes on and 20 minutes off. Heat and cold therapy is subjective; what might work well for you may not work for someone else. Stick with what works best for you!
- Balance activity with rest. Don’t over schedule yourself, take breaks throughout the day. People with RA may be more prone to fatigue than others, recognize your limitations.
- Address stress and anxiety. People with RA/chronic pain are more likely to develop depression because of it. Dr. Metgud recommends building a support network of people to reach out to. Reach out to others that are going through pain and help support others who are recently diagnosed.
If you think you may have RA, Dr. Metgud recommends seeing a rheumatologist. Symptoms can include prolonged stiffness in the joints, especially in the morning. While you cannot reverse joint damage from RA, you can prevent more damage from occurring by following Dr. Metgud’s advice.
Sheela Metgud, MD, sees patients at Illinois Bone & Joint Institute’s Morton Grove and Wilmette locations. To schedule online, please call 847-375-3000 or Schedule online. Learn more about rheumatology at IBJI.
*This content is for information only and is not intended to replace the diagnosis, treatment, or medical advice from your treating healthcare professionals. The content does not provide medical advice, does not constitute the practice of medicine or other healthcare professional services, and does not create a doctor-patient relationship. You should not rely on this information as a substitute, nor does it replace professional medical advice, diagnosis, or treatment. If you have concerns or questions, seek the advice of your healthcare professionals. If you think you may have a medical emergency, call your doctor or 911 immediately. Do not rely on electronic communications or communicate through this website for immediate, urgent medical needs. This website is not designed to facilitate medical emergencies. The use of the information is at the reader’s own risk. The links are provided for information and convenience only. We cannot accept responsibility for the sites linked or the information found here. A link does not imply an endorsement of a site.




