Many patients who have neck or low back pain believe that getting an MRI (CT scan) will pinpoint exactly where the pain is coming from. This, unfortunately, is a common misconception. IBJI’s Dr. Mehul Garala, Physical Medicine and Rehabilitation Physician with Fellowship Training in Spine and Sports Medicine, explains MRI misconceptions when it comes to back pain. (Read Low Back Pain in the Setting of COVID-19)
MRIs are anatomical studies, not pain studies. They evaluate the structures of the spine by producing a series of pictures. However, these structures (such as a disc or a spinal joint) do not stay the same shape and size throughout our lives. They undergo adaptive, age-related changes and MRIs reflect that.
Such a change that can occur is a bulging disc, which has now been proven from multiple studies to be a typical age related finding. The more we age, the more common these findings. They are typical, can be asymptomatic, and do not necessitate treatment. Think of them similarly as if you were to get a gray hair or a wrinkle in your skin. That is why MRI terms such as, “bulging disks, disc desiccation, spondylotic changes, facet arthrosis, endplate spurring, foraminal/lateral recess/central canal narrowing or stenosis” need to be interpreted with caution, because they are common findings as reflected in the table below.
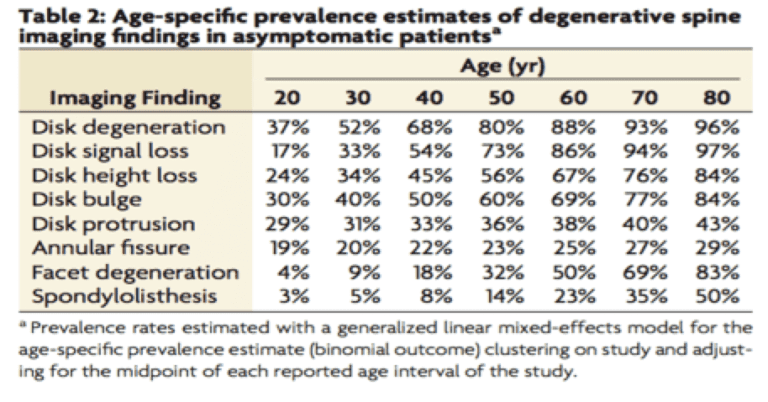
Degenerative Spine Imaging Findings Chart
It is important to understand that MRIs need to be clinically interpreted in the context of the patient’s history and physical exam. The history and physical exam can help the doctor assess if a particular MRI finding can be contributing to the patient’s pain and needs to be addressed, or if it is a typical age-related or incidental finding. This is similar to a mechanic who inspects your car and finds subtle changes to the engine, fluids, brakes, etc. Certain changes, such as minor wear to the brakes might not warrant any intervention such as getting them replaced. The mechanic might think that is an expected finding given the age of the car and it isn’t really impacting the function or its safety. The doctor needs to take a similar approach and determine if a particular MRI finding warrants treatment.
Sources:
Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. Brinjikji, et al. AJNR Am J Neuroradiol. 2015. April.

Mehul Garala, MD
Mehul Garala, MD, is a double board-certified, fellowship-trained physician specializing in Physical Medicine and Rehabilitation, and Sports Medicine, with special interest in non-operative spine management. He performs musculoskeletal and spine evaluations, fracture management, and administers peripheral joint as well as interventional spinal injections.
*This content is for information only and is not intended to replace the diagnosis, treatment, or medical advice from your treating healthcare professionals. The content does not provide medical advice, does not constitute the practice of medicine or other healthcare professional services, and does not create a doctor-patient relationship. You should not rely on this information as a substitute, nor does it replace professional medical advice, diagnosis, or treatment. If you have concerns or questions, seek the advice of your healthcare professionals. If you think you may have a medical emergency, call your doctor or 911 immediately. Do not rely on electronic communications or communicate through this website for immediate, urgent medical needs. This website is not designed to facilitate medical emergencies. The use of the information is at the reader’s own risk. The links are provided for information and convenience only. We cannot accept responsibility for the sites linked or the information found here. A link does not imply an endorsement of a site.




